Efficacy of High-Intensity Resistance and Impact Training (HiRIT) in a Postmenopausal Woman with Osteopenia and Severe Scoliosis: A Preliminary Case Study
Purpose: This preliminary case study examines the safety and efficacy of high-intensity resistance and impact training (HiRIT) in a postmenopausal woman (CS1) diagnosed with osteopenia and severe scoliosis.
Case Description: CS1 is a 62-year-old woman who is 12 years postmenopausal and presents with a double-curved scoliosis, last measured in 2023, showing a Cobb angle of 72 degrees. Prior to starting the exercise program, she had undergone three Prolia® injections.
Baseline Measurements: At baseline, a DXA scan of the lumbar spine (LS) (L1-L2) revealed a T-score of -2.2 and a Z-score of -0.1, corresponding to a bone mineral density (BMD) of 0.800 g/cm². The left hip neck of femur (FN) showed a T-score of -2.4 and a Z-score of -0.9, with a BMD of 0.640 g/cm². The total hip (TH) had a T-score of -1.9 and a Z-score of -0.7, indicating osteopenia. Additionally, a series of functional tests were conducted to assess baseline muscle strength, mobility, and balance.
Treatment Intervention: The HiRIT program comprised private sessions, each lasting 40 minutes. The client participated in these sessions 1 to 2 times per week over a total of 15 weeks, completing 20 sessions. The program included modified lifts, as well as impact and balance exercises specifically tailored to meet the subject's individual needs.
Results: The repeat DXA results for BMD of both LS and the left hip were not able to be directly compared to show the possible effect of the treatment intervention, as the client was retested at a different radiology centre. All functional tests showed improvement ranging from 8 to 28 percent when compared to baseline measurements.
Conclusions: This preliminary case study indicates that HiRIT can be safely and effectively implemented in a postmenopausal woman with osteopenia and severe scoliosis. Additionally, it underscores the critical importance of using consistent Bone Mineral Density (BMD) measurements, preferably with the same equipment at the same radiology clinic. This approach is essential in order to accurately assess the effectiveness of interventions aimed at increasing BMD.
Recommendations: Further research is essential to explore the long-term effects of HiRIT and to establish optimal training protocols within a larger population. Additionally, studies should ensure that the same imaging machine is used for follow-up assessments to maintain consistency in results. Future investigations could also focus on the effectiveness of combining HiRIT with scoliosis-specific exercises in postmenopausal women with low bone mineral density (BMD).
INTRODUCTION
High-intensity resistance impact training (HiRIT) has been shown to be an effective intervention to improve BMD and functional measurements in postmenopausal women and men over the age of 50 with low or very low bone density1,2. However, there are no currently published research studies on the safety or efficacy of a HiRIT intervention in postmenopausal women with osteopenia and severe scoliosis.
CASE DESCRIPTION
A 62 year-old woman, 12 years post menopausal, with a double-curved scoliosis last measured in November 2023 with a Cobb angle of 72.9 degrees from T9 to L3. Lateral and posterior X rays (Image 1 and 2) demonstrate the severe degree of scoliosis (Cobb angle greater than 60 degrees).
Historically, the client’s BMD was closely monitored with repeat DXA scans dating back to 2013. Table 1a demonstrates the BMD scores for L1-L2 and Table 1b the BMD scores for TH from 2013 to 2023. The client commenced Prolia® (3 injections) prior to starting the HiRIT exercise programme.
Table 1a: DXA results for L1-L2
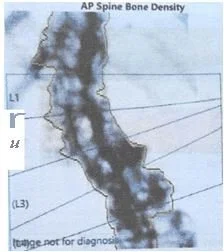
Image 3 below illustrates the difficulty of accurately measuring the BMD in the lumbar spine in cases of severe scoliosis.
Image 3: DXA Lumbar Spine
Table 1b: DXA results for left hip (FN)
BASELINE MEASUREMENTS
Baseline measurements included the most recent DXA results as well as a series of functional tests to measure muscle strength, mobility, and balance.
Baseline DX
The baseline DXA results for Lumbar spine, Left hip (FN and TH) are presented in Table 2.
Table 2: Baseline DXA results for Lumbar spine L1-L2, Left hip (FN and TH) indicating osteopenia.
Baseline Functional Tests
A series of functional tests assessed muscle strength, mobility, and balance. Table 3 provides a description of each test.
Table 3: List and description of functional tests
The following table (table 4) presents the baseline functional test results.
Table 4: Functional test results at baseline.
METHODS
The HiRIT exercise intervention included 3 modified weightlifting techniques, impact exercises and balance activities (see Photos 1-3).
Photo 3: Example of a balance exercise: standing on one leg with an unstable base.
The exercises progressively increased in intensity and difficulty over the course of the program according to the subjects capabilities. Graph 1 shows the progression of the weights lifted by the subject over the first 3 months of her treatment. The HiRIT programme consisted of private sessions of 40 minutes in duration and the client attended 1-2 times a week for 15 weeks (20 sessions in total).
Graph 1: Outlines the weight progression for the client for the 3 lifts
RESULTS
DXA
A bone density DXA was retested on the 17th of March 2025, 3 months after commencing HiRIT. The results are shown in Table 5 below.
Table 5: Repeat DXA
The subsequent DXA scan was performed at a different radiology center, utilizing the same brand of DXA machine (GE Lunar). This report analysed L1-L4, unlike the previous reports which reported levels L1-L2.
Functional Tests
Table 6 compares the functional tests at baseline and at their 3-month retest.
Table 6: Comparison of Functional Tests at baseline and at 3 months.
Nb. All functional tests improved.
The following graph (graph 2) shows the percentage improvement in all functional tests. Increases ranged from 8% for the functional reach to 28 % for the tandem walk..
Graph 2: Functional Tests Percentage Change - Baseline to Post-Treatment Intervention
DISCUSSION
DXA
It was disappointing that at the client's 3-month follow-up, the post treatment DXA was completed at a different clinic, utilizing a different DXA machine, and a change in the region of interest (L1-L2 was changed to L1-L4). Consequently, the DXA results post treatment for all areas {(L1-L2, left hip (FN and TH)} could not be compared to the baseline DXA measures.
As measuring BMD in individuals with severe scoliosis presents challenges, it may be advisable to include other regions of interest not affected by the scoliosis - such as the right hip or radius.
Functional Tests
Post-treatment, the subject showed improved functional test scores. Balance, a major fall risk factor, improved by 28% (tandem walk) and single leg stance by 10% (left) and 13% (right). Functional reach improved 8%, indicating enhanced stability and dynamic posture. This improved balance directly reduces fall risk, increasing safety and confidence3.
Beyond these specific measures, her functional mobility and general walking ability also saw a notable improvement of 14%, as measured by the Timed Up and Go (TUG) test. The TUG test assesses multiple aspects of mobility, including balance, gait speed, and the ability to change direction. The improvement in this score indicates a more efficient and safer movement pattern during everyday tasks, ultimately improving her quality of life and functional independence.
The tragus to wall measurement improved 16% or 24mm which can lead to reduced strain on the neck and back muscles, and importantly in the case of severe scoliosis, an improved respiratory function, as proper alignment can enhance lung capacity4.
These combined improvements underscore the positive impact on her ability to perform daily activities with greater ease, stability, safety and confidence.
Treatment Variables
It is important to note that the client was provided with a multi-treatment approach: regular DXA tests to monitor the trend of BMD, bone medication (Prolia®), bone health education regarding modifiable risk factors such as diet, supplements such as Vitamin D as well as commencing a HiRIT exercise programme. As treatments were combined we are unable to state categorically which treatment intervention was responsible or contributed to any changes in the functional tests.
CONCLUSION
In this case study the effect of HiRIT on BMD could not be ascertained. This case study reinforces the importance of using the same DXA machine for continuity, thereby ensuring an accurate comparison and interpretation of treatment interventions. Post treatment assessment showed improvements in all functional measurements of muscle strength, endurance, balance, flexibility and agility without injury. Improvement in these tests have been shown to greatly reduce the possibility of falls and fracture risk1,2.
This preliminary case study is a starting point for further research in this growing demographic. Future studies should aim to involve group participation in order to provide a more economical treatment approach as well as to enhance the reliability and validity of the results. Combining bone building exercises with a form of Physiotherapy Scoliosis Specific Exercises (PSSE) would also be a very interesting project as there is currently no research available to ascertain the benefits of a combined exercise approach on BMD.
Limitations
A preliminary case study of N=1 has inherent limitations such as: the findings cannot be generalised to the larger population, without a comparison group, it’s challenging to determine whether the observed effects are due to the HiRIT intervention or other factors and, statistical analysis is limited to descriptive statistics only.
References:
1. Watson SL, Week BK, Weis L, Horan SA, and Beck BR. (2018). High-Intensity Resistance and Impact Training Improves Bone Mineral Density and Physical Function in Postmenopausal Women With Osteopenia and Osteoporosis: The LIFTMOR Randomized Controlled Trail. Journal Bone Mineral Research 33(2):211-220.
2. Watson SL, Week BK, Weis L, Horan SA, and Beck BR. (2015). Heavy Resistance Training is Safe and Improves Bone, Function and Stature in Postmenopausal Women with low to very low Bone Mass: Novel Early Findings from the LIFTMOR Trial. Osteoporosis International 26(12) 2885-2894.
3. Ward, RE, Leveille SG, Beauchamp, MK, Travison, T, Alexander, N, Jette, AM, and Bean, JF. Functional Performance As a Predictor of Injurious Falls Among Older Adults. J Am Geriatr Soc. 2015 Feb;63(2):315-320.
4. Han,j, Park, S, Kim, Y, Choi, Y and Lyu,H. Effects of Forward Head Posture on Forced Vital Capacity and Respiratory Muscles Activity. J Phys Ther Sci. 2016 Jan 30;28(1):128-131.
Acknowledgements: The author would like to sincerely thank the subject for allowing her case to be presented.