Unlocking Your Potential: Amanda's Guide to Flexor Hallacis Longus Tendinopathy
Understanding Flexor Hallucis Longus Tendinopathy (FHL)
Have you been struggling with pain, limited movement, or discomfort in your inner ankle and foot, that you were told it could be the Achilles or Plantarfasciitis, but not quite after you google the symptoms online? You may be experiencing a common condition known as Flexor Hallucis Longus (FHL) Tendinopathy. While it can be frustrating, understanding what's happening in your body is the first step toward recovery.
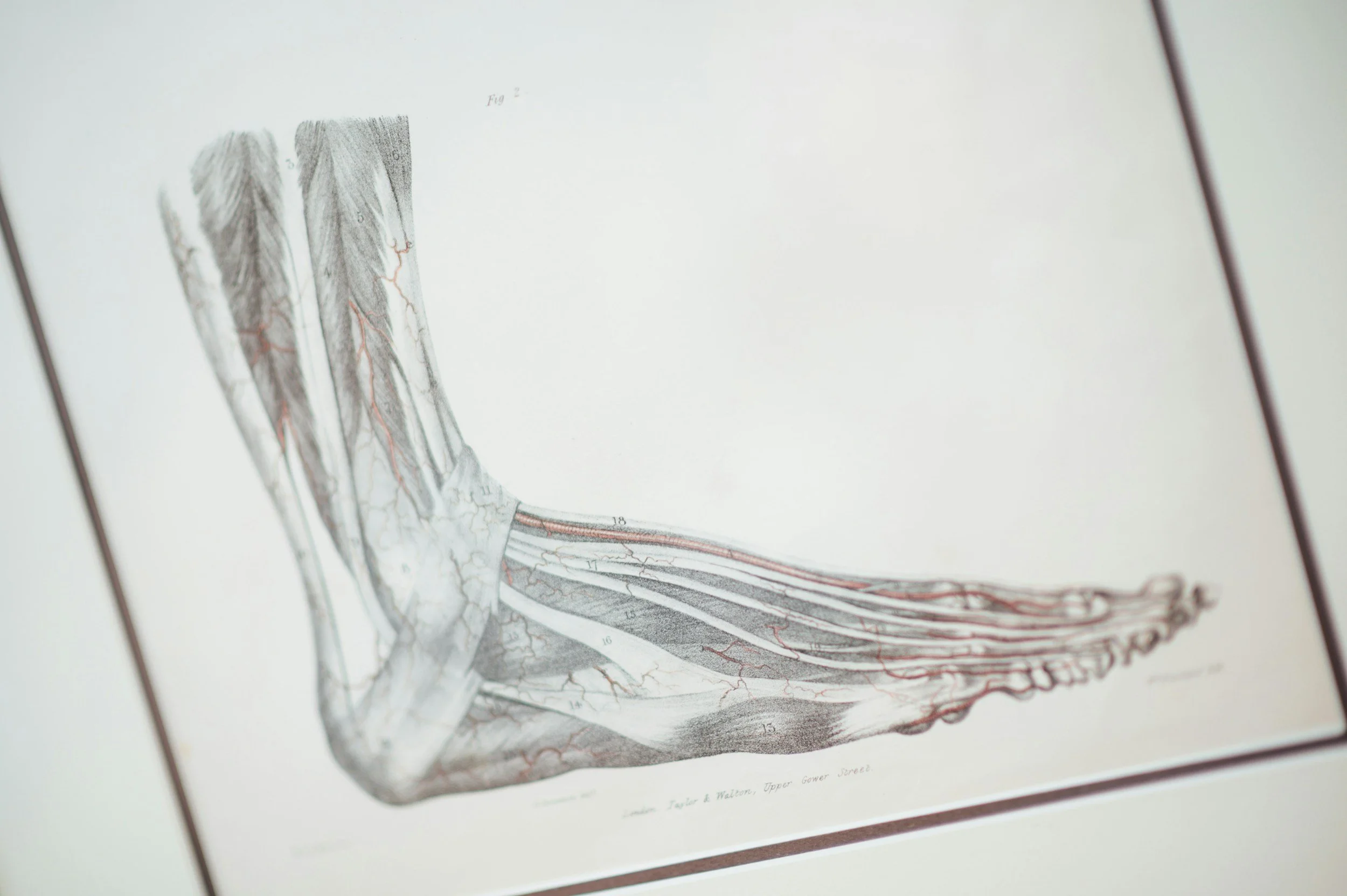
Flexor hallucis longus is the main muscle that flexes the big toe and assists plantarflexing (pointing) the ankle. It runs from the deep layer of the leg, passes through the back of the inner ankle bone (medial malleolus), runs along the longitudinal arch of the foot and attaches to the big toe.
People with FHL tendinopathy usually presents with pain along the course of the muscle/tendon, and worse with toe-off during walking/running, and landing from jumps. It is usually associated with an overuse mechanism: repetitive plantarflexion (pointing) of the ankle, or wearing shoes that are too big that requires “toe-grip” to keep the foot in place in the shoe.
FHL tendinopathy limits people from performing daily activities (e.g. walking) as well as performing their sports (e.g. running and dancing) due to pain. It may also be an indicator of weak muscles or poor stability/mobility of the structures around.
The Role of Physiotherapy in Treatment
Many people wonder if physiotherapy can truly help with FHL tendinopathy. The short answer is, absolutely! Our goal isn't just to treat the symptoms but to address the root cause. A physiotherapist can help by:
Accurate Diagnosis: Performing a thorough assessment to pinpoint the exact cause of your pain.
Pain Management: Using techniques like manual therapy, dry needling, or electrotherapy to reduce your discomfort.
Improving Mobility: Using manual therapy (e.g. joint mobilisation) to restore joint movements, and prescribing targeted exercises to maintain range of motion and regain flexibility.
Building Strength: Developing a personalized strengthening program to support the affected area and prevent future injury.
Patient Education: Providing you with the knowledge and tools to manage your condition and maintain a healthy, active lifestyle.
A Patient's Journey: JQ's Story
To show you what this looks like in practice, I want to share the story of one of my patients.
The Initial Challenge
My Patient came to see me with an initial lateral ankle sprain injury. They were struggling with weightbearing on that foot without pain and was walking with a significant limp. As the ankle sprain recovers, JQ reported pain on the inside of the ankle. This was limiting their ability to walk between places, and preventing them from playing tennis and pickleball, and wearing the shoes they like without pain.
Our Collaborative Treatment Plan
We started with a comprehensive assessment to understand their specific needs. Our plan included:
Phase 1: Pain Reduction. We focused on calming the painful area with therapeutic ultrasound, gentle joint mobilisation and soft tissue release.
Phase 2: Restoring Movement. Once the pain was more manageable, we introduced a series of exercises to regain their range of motion, like ankle alphabets and weight-bearing ankle dorsiflexion mobilisation with movement (MWM).
Phase 3: Strengthening and Prevention. To build resilience and prevent a recurrence, we progressed to balancing and strengthening exercises, such as single-leg-stance with external perturbation, toe yoga and calf raises with ball between ankles.
The Outcome
After four weeks of consistent work, JQ made incredible progress. They are now able to return to playing pickleball and wear their regular shoes without issues. Their story is a powerful reminder that with the right guidance and a little dedication, recovery is within reach.
Ready to Start Your Journey? Book A Session With Amanda Today!
If you're dealing with FHL tendinopathy, don't wait for the pain to go away on its own. Reaching out to a physiotherapist can be the turning point in your recovery. We're here to help you get back to doing the things you love, without being held back by pain.